Optimizing IBD Treatment with Key Nutritional Strategies
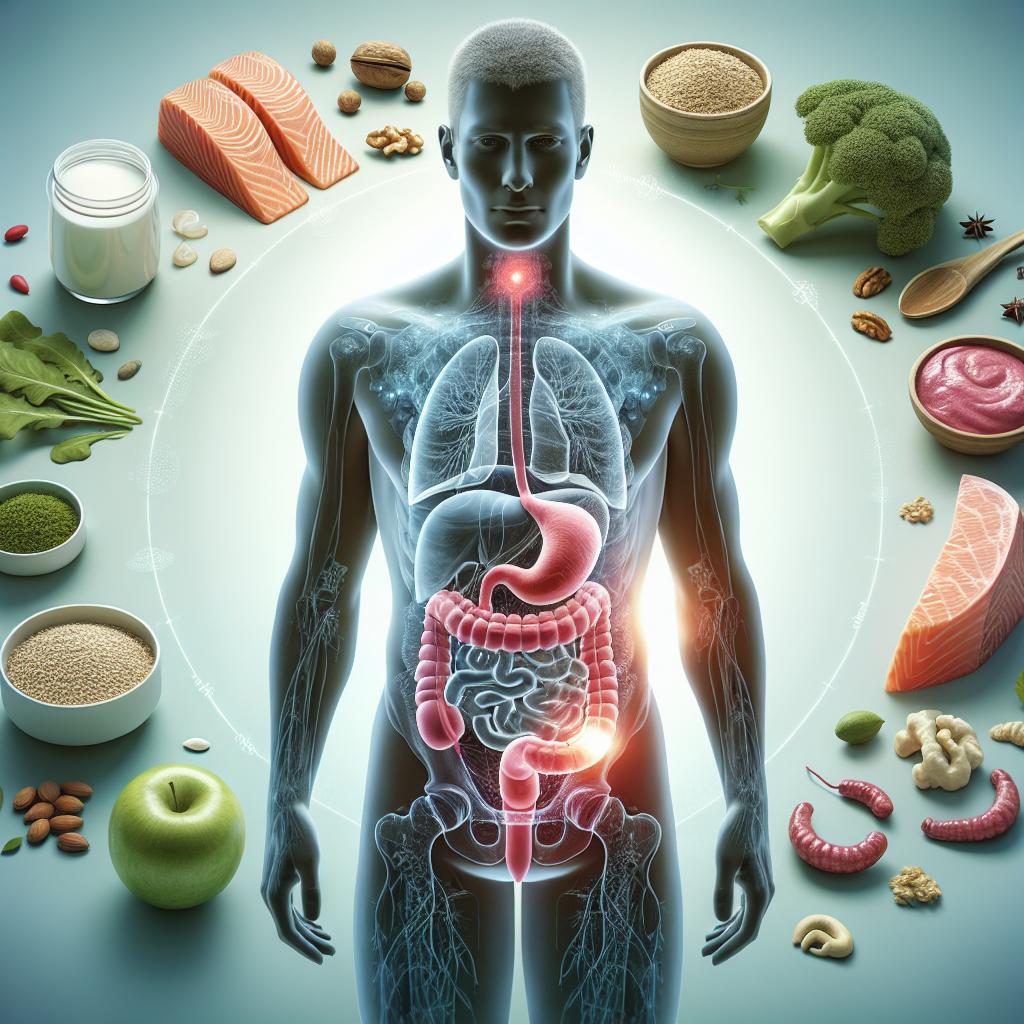
Living with Inflammatory Bowel Disease (IBD) presents unique challenges. Patients often struggle with nutrient absorption while managing painful symptoms. Nutrition plays a critical role in both disease management and overall well-being for IBD patients.
Recent research shows that targeted nutritional strategies can significantly improve outcomes for those with Crohn’s disease and ulcerative colitis. Let’s explore how dietary approaches can complement medical treatments to optimize IBD management.
Understanding the Nutritional Challenges in IBD
IBD creates a perfect storm of nutritional problems. The inflammation damages the intestinal lining, which reduces nutrient absorption. Also, symptoms like diarrhea and abdominal pain often lead to reduced food intake.
Additionally, many IBD medications affect nutrient levels in the body. For example, corticosteroids impact calcium metabolism while sulfasalazine can interfere with folate absorption. These factors combine to create significant nutritional deficiencies.
Common nutritional deficiencies in IBD patients include:
- Iron (leading to anemia)
- Vitamin D and calcium
- B vitamins, especially B12
- Zinc
- Magnesium
- Protein
Dr. Maria Abreu, Director of the Crohn’s and Colitis Center at the University of Miami, explains: “Nutrition in IBD is both a science and an art. Each patient needs individualized assessment and regular monitoring as their disease evolves.” This personalized approach is key to successful nutritional management.
Evidence-Based Dietary Approaches for IBD
Several dietary strategies have shown promise for IBD management. These approaches aim to reduce inflammation, improve nutrient absorption, and maintain remission.
Exclusive Enteral Nutrition (EEN)
EEN involves consuming a liquid formula as the sole source of nutrition for a defined period. This approach has shown remarkable results, especially for Crohn’s disease.
Studies show that EEN induces remission in up to 80% of pediatric Crohn’s patients. Furthermore, it promotes mucosal healing without the side effects of medications like corticosteroids.
The formula typically provides complete nutrition while eliminating potential food triggers. After the initial treatment period (usually 6-8 weeks), foods are gradually reintroduced while monitoring symptoms.
The Specific Carbohydrate Diet (SCD)
The SCD restricts complex carbohydrates and processed foods. It’s based on the theory that these foods feed harmful gut bacteria that contribute to inflammation.
This diet allows simple carbohydrates, most proteins, and healthy fats while eliminating grains, most dairy, and added sugars. Many IBD patients report symptom improvement on the SCD, though more research is needed to fully validate its effectiveness.
A 2017 study in the Journal of Clinical Gastroenterology found that the SCD improved symptoms and inflammatory markers in pediatric Crohn’s patients. However, the diet requires significant commitment and careful planning.
The Mediterranean Diet
The Mediterranean diet emphasizes olive oil, fruits, vegetables, whole grains, and fish. This eating pattern delivers anti-inflammatory benefits through its rich polyphenol content.
Research suggests this diet may help maintain remission in IBD. The high fiber content also promotes a healthy gut microbiome, which plays a crucial role in immune function.
Adapting the Mediterranean diet for IBD may require some modifications. For example, patients may need to cook vegetables thoroughly and temporarily limit high-fiber foods during flares.
Key Nutrients for IBD Management
Beyond broad dietary approaches, certain nutrients deserve special attention in IBD management.
Omega-3 Fatty Acids
Omega-3s possess powerful anti-inflammatory properties. Cold-water fish like salmon, mackerel, and sardines provide excellent sources of these beneficial fats.
While research shows mixed results on omega-3 supplements for IBD, including fatty fish in the diet appears beneficial. For those who don’t consume fish, plant sources like flaxseeds and walnuts offer alternative options.
Vitamin D
Vitamin D deficiency affects up to 70% of IBD patients. This nutrient plays a crucial role in immune regulation and bone health.
Regular testing and supplementation often prove necessary for IBD patients. Evidence suggests that maintaining optimal vitamin D levels may help reduce inflammation and improve disease outcomes.
Probiotics and Prebiotics
Gut bacteria influence IBD development and progression. Certain probiotic strains show promise for ulcerative colitis management, particularly VSL#3 and E. coli Nissle 1917.
Prebiotics feed beneficial gut bacteria and include foods like bananas, onions, and asparagus. However, some IBD patients may not tolerate these high-FODMAP foods during flares.
The best approach involves working with a healthcare provider to find appropriate probiotic strains and prebiotic foods based on individual tolerance.
Practical Nutrition Strategies During Flares and Remission
Nutritional needs change dramatically based on disease activity. Adapting dietary strategies accordingly helps manage symptoms and maintain optimal nutrition.
During Flares: Reducing Digestive Workload
When IBD symptoms flare, the digestive system needs gentle support. Consider these strategies:
- Choose low-fiber, easy-to-digest foods (white rice, bananas, well-cooked vegetables)
- Consume smaller, more frequent meals
- Stay hydrated with water, broth, and electrolyte solutions
- Consider liquid nutrition supplements to maintain calorie and protein intake
- Avoid potential trigger foods like dairy, spicy foods, and caffeine
During severe flares, working with a dietitian to develop a temporary elemental or semi-elemental diet may help reduce inflammation while providing essential nutrition.
During Remission: Building Nutritional Reserves
Periods of remission offer opportunities to improve nutritional status. Focus on these approaches:
- Gradually increase dietary diversity to expand nutrient intake
- Incorporate more fiber-rich foods to support gut microbiome health
- Emphasize nutrient-dense foods to replenish depleted stores
- Address specific deficiencies through targeted foods or supplements
- Keep a food journal to identify personal trigger foods
This balanced approach helps build nutritional reserves while maintaining symptom control. Remember that what works varies greatly between individuals with IBD.
The Role of Nutritional Supplementation
While whole foods provide the best nutrition, supplements often become necessary for IBD patients. Common supplement needs include:
- Multivitamin/mineral: to address multiple deficiencies
- Iron: for anemia prevention and treatment
- Calcium and vitamin D: for bone health
- B12: especially for those with ileal involvement or resection
- Zinc: often depleted due to diarrhea and poor absorption
However, not all supplements are beneficial. Some may contain additives that trigger symptoms or interact with medications. Always consult healthcare providers before starting supplements.
Registered dietitian Kelly Issokson, MS, RD, from the Cedars-Sinai Inflammatory Bowel Disease Center, advises: “Supplement quality matters tremendously for IBD patients. Look for products free from fillers, artificial colors, and common allergens that might trigger symptoms.”
Building Your Personalized IBD Nutrition Plan
Creating an effective nutrition plan requires a team approach. Here’s how to develop your strategy:
Assemble Your Support Team
An ideal IBD nutrition team includes:
- Gastroenterologist: to monitor disease activity and medication effects
- Registered dietitian: preferably one specializing in IBD
- Primary care provider: to address overall health needs
- Mental health professional: for addressing food anxiety and diet-related stress
This collaborative approach ensures comprehensive care addressing all aspects of nutritional health.
Track and Monitor Your Response
Keeping detailed records helps identify patterns and guide adjustments. Consider tracking:
- Food intake and any symptom responses
- Bowel movements and pain levels
- Energy levels and other quality-of-life measures
- Weight changes
- Laboratory values from regular testing
Many mobile apps now facilitate this tracking process. Sharing this information with your healthcare team improves treatment decisions.
Adjust Based on Disease Changes
IBD is dynamic, requiring ongoing nutritional adaptations. Regular reassessment ensures your approach remains effective as your condition changes.
This flexibility proves especially important during disease transitions, medication changes, or after surgical interventions. Each situation may require different nutritional strategies.
Beyond Diet: Comprehensive Nutrition Support
Complete nutritional care extends beyond food choices. Additional considerations include:
Medication-Nutrient Interactions
Many IBD medications affect nutrient levels. For example:
- Corticosteroids increase calcium needs
- Methotrexate requires additional folate
- Sulfasalazine can reduce folate absorption
- Antibiotics may disrupt gut flora
Understanding these interactions helps prevent additional deficiencies. Timing medications and meals appropriately can also improve both drug effectiveness and nutrient absorption.
Addressing Malabsorption
For patients with significant malabsorption, specialized approaches may help:
- Medium-chain triglyceride (MCT) oil provides easily absorbed fats
- Pancreatic enzymes may improve nutrient digestion
- Injectable forms of nutrients bypass the digestive system when needed
- Enteral or parenteral nutrition supports those unable to maintain nutrition orally
These interventions require medical supervision but can dramatically improve nutritional status in severe cases.
The Future of Nutrition in IBD Care
Exciting developments are emerging in nutritional approaches to IBD. Research areas include:
- Personalized nutrition based on genetic profiles
- Targeted prebiotics to optimize individual microbiomes
- Novel food processing techniques that reduce inflammatory potential
- Digital tools for real-time symptom and nutrition tracking
These advances promise more effective, individualized nutritional approaches for future IBD management.
Conclusion: Empowering Yourself Through Nutrition
Nutrition represents a powerful tool for IBD management. While it can’t replace medical therapy, optimized nutrition significantly enhances treatment outcomes and quality of life.
By working with healthcare providers, tracking your responses, and adapting to your body’s changing needs, you can harness nutrition’s power in your IBD journey. Remember that patience and persistence are essential—finding your optimal nutritional approach takes time.
Have you found specific nutritional strategies helpful for your IBD management? Consider discussing them with your healthcare team to incorporate them into your comprehensive treatment plan.
References
- Crohn’s & Colitis Foundation: Diet and Nutrition
- Journal of Clinical Gastroenterology: Specific Carbohydrate Diet for Pediatric Inflammatory Bowel Disease
- National Institute of Diabetes and Digestive and Kidney Diseases: Eating, Diet, & Nutrition for IBD
- Gastroenterology: Current Directions in IBD Therapy
- University of Alberta IBD Clinic: Nutrition Resources


